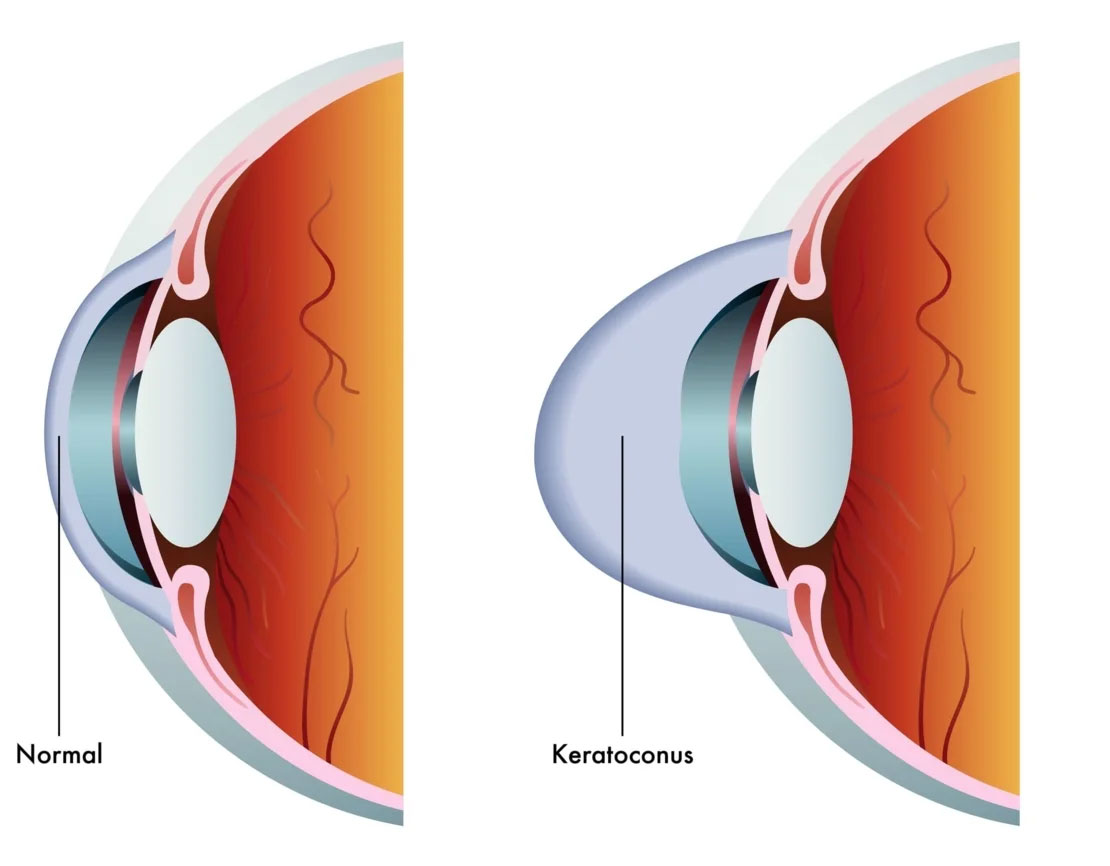
Keratoconus is an eye condition in which the shape of the cornea becomes distorted.
Keratoconus is an eye condition in which the shape of the cornea becomes distorted. The cornea is a clear structure that covers the front of the eye and allows light to enter the eye. In a healthy eye, the cornea curves like a dome. In an eye with keratoconus, the center of the cornea slowly thins and bulges so that it sags and has a cone shape.
Living with KeratoconusThe cause of keratoconus is unknown.
Keratoconus tends to affect younger people and the symptoms sometimes start in the early teen years and progresses most rapidly for the next 10 to 20 years. Often, eyeglass prescriptions must be changed frequently as the disease progresses.
Symptoms include:
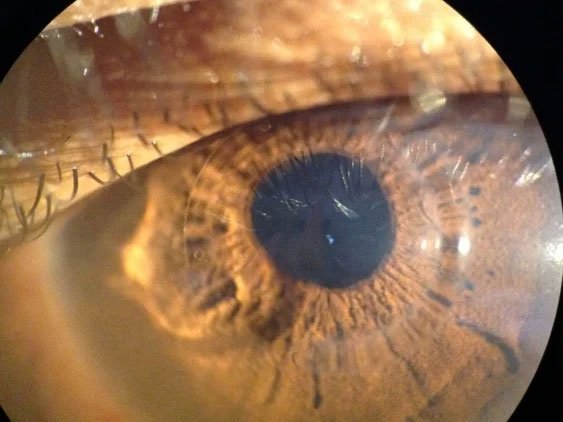
Keratoconus can usually be diagnosed with a slit-lamp examination as well measurement of the corneal curvature. Your optometrist will look for signs such as corneal thinning, stress lines, and scarring at the apex of the corneal cone. Keratoconus, especially in the early stages, can be difficult to diagnose and its symptoms could be associated with other eye problems. Simply recognizing symptoms does not by itself diagnose the condition.
The primary treatment options for keratoconus have traditionally been contact lenses and surgery. In the very early stages of keratoconus, vision problems can be corrected with prescription glasses or contact lenses. As keratoconus progresses, special rigid gas permeable contact lenses may be necessary.
Collagen Cross-Linking is a new exciting treatment that has been shown to halt the progression of the keratoconic changes that happen in the cornea. By combining specially formulated Riboflavin and carefully engineered ultraviolet light therapy, patients with keratoconus finally have a treatment that has halt the disease, and may even improve their vision.
INTACS corneal inserts and Kera-rings are designed to help patients with keratoconus that have become contact lens intolerant. Clinical results have shown both improved lens free as well as lens-wearing vision improvement, and many patients do not necessarily go on to needing a corneal transplant.
Advanced keratoconus, with scarring and thinning of the corneal tissue may require surgery. A full thickness corneal transplant is often performed in a hospital setting, on an outpatient ambulatory basis. Surgery is usually less than an hour.
Please contact the office to make an appointment so that Dr Ehrenhaus can examine you and help advise you with the best options available for your individual needs.
In addition to traditional treatments, we now offer Corneal Allogenic Intrastromal Ring Segments (CAIRS) — a cutting-edge procedure for appropriate keratoconus patients who are seeking increased visual stability and comfort.
With CAIRS, ultra-thin ring segments made from donor corneal tissue are placed into a specially prepared channel within your own cornea. These natural implants reshape the corneal curvature and help reduce the bulging and irregular astigmatism characteristic of keratoconus. Because the segments are derived from human tissue rather than synthetic material, there is a potential for greater biocompatibility and long-term stability.
We perform a comprehensive evaluation including corneal topography, thickness mapping, and vision testing to determine candidacy. Ideal candidates are patients with progressive ectasia or keratoconus, who may experience contact-lens intolerance or increasing lens changes, and who wish to explore alternatives to more invasive surgery.
If you’re managing keratoconus and wish to learn whether CAIRS may be a proper option for you, please schedule a consultation at our office. We’ll review all available treatments and tailor a plan designed specifically to your cornea and visual goals.
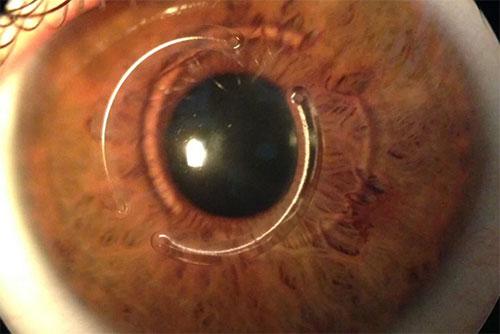
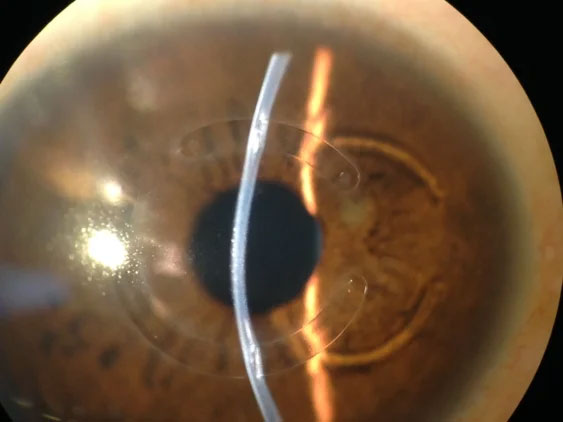
KERARING, intrastromal corneal ring segments, offer a minimally invasive approach for corneal remodeling, the treatment of keratoconus, and other ectatic corneal disease. As the most complete and versatile corneal remodeling system available today, KERARING implants are available in variable arc lengths, thicknesses, and diameters. They offer a high level of customization to remodel the corneal surface while reducing refractive errors associated with keratoconus and other ectatic corneal disorders. With implantation, the KERARING segments adjust the cone back in line with the rest of the cornea, regularizing corneal topography and stabilizing corneal ectasia. They offer an effective treatment for managing keratoconus while preventing or delaying the need for more invasive approaches to care.
Placing KERARING segments involves a quick and minimally invasive laser procedure, allowing patients to resume their normal activities soon afterward. Typically performed as an outpatient procedure, the resulting topographic and refractive changes start right away, generally stabilizing three months after treatment. It's also reversible if vision changes or the results indicate a need to remove the implants.
Learn MoreDr. Ehrenhaus using the latest Femtosecond Laser, designed by Zeimer (Swiss) to implant KERATACx Corneal Rings for Keratoconus and to create bladeless LASIK flaps.
The keratoconus patients implanted with Keratracx corneal ring implants were already noticing up to 2-3 lines of vision improvement without glasses or contacts the next day!

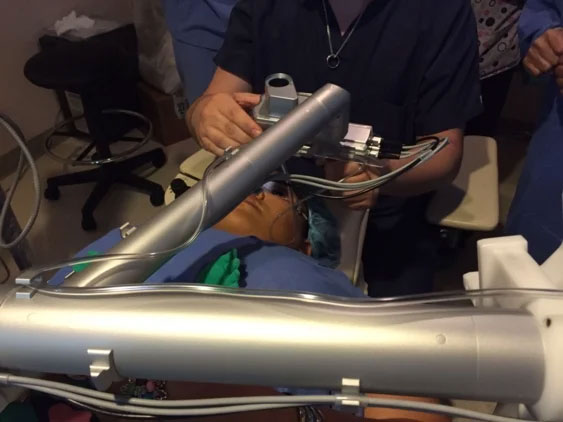



The patient had an easy uncomplicated recovery after the 10 minutes procedure and is already seeing better without his RGP lenses than with them!